Endodontic treatment #17: Management of medium-large canals
September 2, 2025
|
A 22-year-old female patient presented with pain upon biting and a persistent dull ache in the area of tooth #17. The patient had no significant medical history. Clinical examination of the vestibular and palatal areas in the first quadrant showed no visible signs of swelling ,redness, or fistula formation. Palpation was also negative. Periodontal probing depths did not exceed 3
mm. Teeth numbers #15, #16, and #17 had previously been treated with composite fillings by another dentist. Only tooth #17 tested negative for vitality and positive on percussion. An intraoral X-ray was performed, showing a deep filling and signs of periapical radiolucency on tooth #17 (Fig. 1). Based on these findings, pulpal necrosis was identified as the cause of the symptoms, with chronic apical periodontitis determined as the main diagnosis. The patient was scheduled for root canal treatment. Due to the complex root canal anatomy, treatment was completed over two appointments. After creating the access cavity, the orifices of the MB1, DB, and P root canals were visualized under dental operating microscope (DOM).

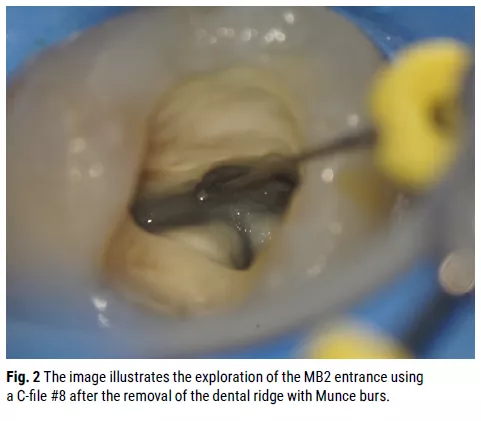
Due to the small radius of curvature in the MB1and DB canals, the glide path was initiated with pre-bent C-files #6, 8, and 10, followed by a K- File #10 to establish the correct glide path. A M4 handpiece was also utilized. The palatal root canal was instrumented initially with a K-File #25. To access MB2, the dental ridge above its entrance was removed using Munce burs. After scouting the entrance with a C-file #8 (Fig. 2), the Traverse glide path file 13/06 was used to achieve a straight-line path, gently brushing mesially without forcing the file apically.
(Fig. 3). Ultimately, a secure glide path was established in all root canals. The MB2 canal showed a connection to MB1 (Vertucci Type II configuration). Throughout the treatment, copious NaOCl irrigation and activation of the solution were performed. Calcium hydroxide dressing, sterile Teflon tape, and an adhesive filling were used to secure the access cavity.

In the second appointment, final preparation was completed with the Traverse glide path 13/.06 file and ZenFlex files: MB1 40/.06, MB2 25/.06 (prepared only to the connection), DB 40/.06, and P 40/.06. Copious NaOCl irrigation and activation of the solution were repeated at each stage. NaOCl was removed and EDTA was left in the root canal system for 5 minutes. NaOCl was used as the final irrigant. A single-cone obturation technique was performed using a calcium-silicate-based sealer. Core build-up with short-fiber reinforced composite was applied, followed by a top layer of composite to restore the correct occlusal morphology. A final intraoral X-ray was taken post-treatment (Fig. 4). The patient was scheduled for a 12-month recall (Fig. 5).


MKT-25-0092-UK Rev-0
Share This









